A Mother’s Fight for Her Son: Why Every Rare Life Deserves a Chance to Breathe
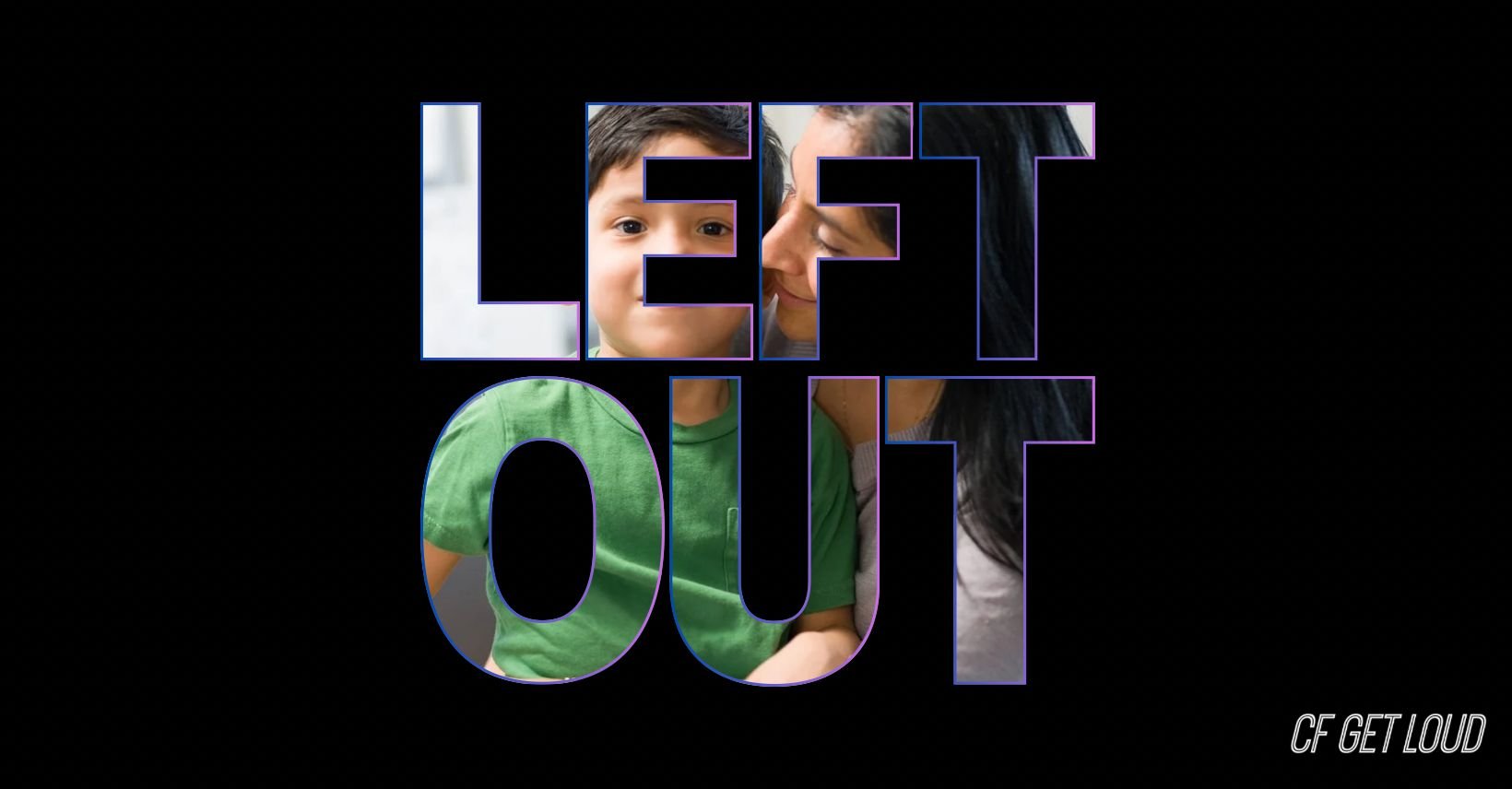
Photo of Vicky and her son, Sebastian. This is one of the many families being left behind by our government.
For many, newborn screening is a beacon of hope—a reassurance that early detection can protect our children from the invisible threats of genetic diseases. In Ontario, every baby undergoes this screening, a vital test to catch serious genetic conditions before symptoms manifest. But for Vicky, this reassurance unraveled into a story of missed diagnoses and a relentless fight for her son’s life.
When Vicky’s twin boys, beautiful and seemingly healthy, were born, she felt a joy that only parents know. But while one of her boys thrived, the other began to show signs that something wasn’t right. Vicky’s maternal instinct pushed her to seek answers. Her baby boy, Sebastian, seemed to struggle with even the mildest colds, while his twin remained robust and healthy. The difference was stark, and she couldn’t ignore it. Why wasn’t this caught by the newborn screening?
A System Designed for the Common, but Not the Rare
Newborn screening in Ontario is designed to test for common genetic variations associated with serious conditions, including Cystic Fibrosis (CF). It’s a powerful tool, but it has limitations. In Vicky’s case, her son Sebastian’s genetic mutations were so rare they slipped through the cracks. One of these mutations is found predominantly in people of Indigenous Andean ancestry, particularly Ecuadorian, reflecting Vicky’s heritage. The other mutation is also rare, not included in the typical screening panels. Sebastian’s case represents an overlooked category in healthcare—ultra-rare patients within already rare diseases.
Sebastian is part of the “Ultra Rare” population within the CF community. For many CF patients, a groundbreaking gene therapy called Trikafta has provided a new lease on life. This treatment doesn’t cure CF, but it slows the disease’s progression, reducing lung infections by up to 60% and giving children back a semblance of a normal childhood. It’s a lifeline—one that allows patients to breathe easier and live longer. But for Sebastian, and those like him, access to Trikafta remains a distant hope.
When “Access” Is a Matter of Genetics
The story takes a hopeful turn when Sebastian is placed under the care of the dedicated team at Sick Kids Hospital. Here, with extensive research and specialized lab programs, his cells were tested to see if Trikafta could help. The results were promising. The lab findings showed that Sebastian’s unique genetic profile could indeed respond well to the therapy.
Just when it seemed like the family could celebrate, they were hit with another devastating blow: Trikafta was not funded for Sebastian’s specific genetic mutation. Despite the scientific evidence, the Canadian model for Trikafta funding only includes specific gene types. Sebastian’s gene type simply wasn’t on the list.
Why Is There a List? When Doctors Believe in a Life-Saving Medicine, Why Can’t They Prescribe It?
This is the question Vicky asks every day. Why should a list determine access to a medicine that could save her son’s life? Why should Sebastian’s life hinge on arbitrary inclusion criteria rather than a doctor’s expertise and evidence of efficacy? If a Cystic Fibrosis specialist believes that Trikafta could give Sebastian the life he deserves, should he not have the right to try it? This is why countless families and supporters have poured their energy, resources, and hope into CF research. We need a cure, but until that day comes, we need access to whatever treatments can prolong and improve lives.
A Call for Change: No One Should Be Left Behind.
Health Canada has approved Trikafta for a list of genetic mutations, but our Canadian population is a beautiful mosaic of backgrounds and ancestries, making every patient unique. The rarest among us deserve the same chance at life, the same opportunity to try.
In Alberta, progress is happening. Recently, the provincial government changed its funding model for Trikafta, giving doctors the power to make treatment decisions based on their professional judgment and the specific needs of each patient. This change puts the decision-making where it belongs—in the hands of the experts who understand the nuances of CF and the potential of Trikafta.
This approach makes sense. CF patients live with a fragile balance of health, undergoing countless medical regimens, physiotherapy, and hospitalizations. They deserve the right to try any treatment that may help them, under the guidance of their doctors.
Thank you, Alberta.
A Plea to Canada: Protect the Right to Breathe
We are calling on all provinces in Canada to follow Alberta’s lead. Every person with CF, no matter how rare their genetic makeup, deserves the right to breathe and the right to try treatments that may change their lives. Vicky’s story, Sebastian’s struggle, and the experiences of so many others remind us that healthcare should be equitable and compassionate. Every life is valuable, and every child deserves the chance to grow, dream, and live fully.
This is more than a plea; it’s a call to action. Raise your voice with us. Let’s demand that our healthcare system protect the rare lives among us. Everyone deserves the right to try, the right to hope, and the right to breathe.